Do you experience hip pain when going up or downstairs? Do you search for the elevator anytime you are in a building to avoid using the stairs because you don’t want the pain in your hip to increase?
This is a common problem, and there are several potential causes. However, pain with stairs is not something you should accept and avoid. There are ways to address your pain and get back to doing stairs pain-free.
This article will discuss the main reasons you would have hip pain with stairs. We will also review how to treat each condition and the steps you need to take to make them feel better.
Why Do Stairs Cause Hip Pain?
Stairs can cause hip pain for a few primary reasons. Once you understand the forces at play with going up and downstairs, the easier it is to understand and fix.
There are a few reasons hip pain and stairs go hand-in-hand. The most common causes are:
- Hip bursitis
- Glute medius tendonitis
- Osteoarthritis
- A hip labral tear
- Lumbar radicular pain
Let’s take a closer look at each one, and then we’ll give a small amount of information on how to address each issue.
Hip Bursitis
The hip is a ball-and-socket joint. This means that the round head of your femur (thighbone) fits snugly into the hip socket. Within our joints are tiny fluid-filled sacs called bursa. These bursa help to lubricate and protect the hip joint while preventing friction between the tendons and bones.
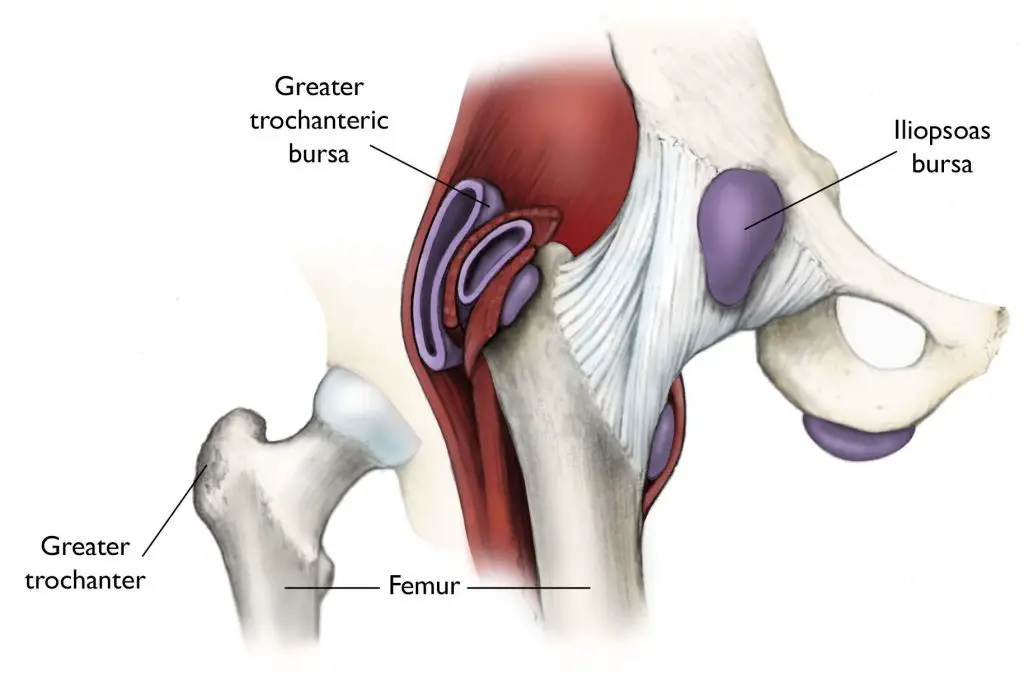
Bursae are sacs filled with fluid that cushions the tendons and bones. There are over 150 bursae in your body, and they are located in areas where tendons or muscles may rub against bone.
Bursitis is a fancy way of saying there is irritation of a bursa. It can be caused by repetitive motions, direct trauma, or an underlying condition such as arthritis. When the bursa becomes inflamed, it can cause pain and stiffness in the hip joint.
How to Address Hip Bursitis
The first step in addressing hip bursitis is modifying or pausing activities that aggravate the bursa. This could be running, sitting for too long, or walking too far in one bout.
Try sleeping on the other side with a knee pillow between your legs to relieve pain at night. We also recommend using heat to bring blood to the bursa to heal for 20 minutes right before bed.
The best way to improve Bursitis is to strengthen the muscles in the immediate area of the bursa. This may seem counterintuitive; however, the stronger the muscles are, the less pressure that walking and stairs will put on the bursa because the muscles will take all the stress.

Glute medius weakness and hip bursitis go hand-in-hand. Glute weakness is a high predictor of future hip bursitis. It may be uncomfortable at first, but strengthening the muscles near the bursitis is necessary to improve your symptoms.
Related Topic: The Best Exercises for Glute Strengthening
Glute Medius Tendonitis
The Glute Medius is a muscle on the outside of your hip. Its primary role is to stabilize the hip and keep us upright with the rest of our body when standing or walking.
Tendonitis is an irritation to the level of small micro-tears in a tendon. Glute medius tendonitis is caused by muscle weakness, which causes excess forces to be transferred to the tendon during activities such as going up and down stairs.
Tendonitis is often misdiagnosed as Bursitis and given a steroid injection which may help with pain temporarily. However, it doesn’t address the real issue, so it’s likely to return in a few months.
How to Address Glute Med Tendonitis
The primary way to fix glute tendonitis is with glute medius and lateral hip strengthening. This builds the tendon up stronger and causes the body to repair the micro-tears within the tendon.
Our favorite ways to address hip weakness are with side-lying clamshells, sidesteps with a mini-loop band, lateral step downs, and reverse mini lunges.
Without an active strengthening program, the micro-tears in the tendon will remain and return the next time you increase your activity.
Related Topic: Our Favorite Ways to Increase Glute Strength
Hip Osteoarthritis
A layer of smooth cartilage covers the ball and socket and cushions them as they move. This is what allows us to have a pain-free hip joint. When this cartilage wears down from overuse, injury, or normal aging, it’s called osteoarthritis (OA).
The hip joint is unique because it experiences a lot of force and movement. The more weight you carry, the greater the risk of developing hip OA.

The first symptom of hip osteoarthritis is typically a slow onset of stiffness that may not even be painful. This loss of motion tends to progress slowly and sneak up on people without them realizing it.
After the slow onset of stiffness, you may feel achy and stiff after rest periods, such as sitting for too long. As the disease progresses, you may have pain even when you are not active, and the only time you get relief is when you are in a non-weight-bearing position.
How to Address Hip Osteoarthritis
You can do things at home to help manage your symptoms, such as using a cane or walker when needed, heat or ice, losing weight if you are overweight, and taking over-the-counter anti-inflammatory medications.
We recommend a 6-week hip strengthening program to help support the hip joint. If the muscles aren’t strong enough, each step places more pressure on the joint’s bones.
There is a good chance that you’ve favored and protected the arthritic hip joint for a long time and have not realized it, so it’s almost a guarantee that there is weakness in the muscles around the joint.
If these things don’t help with your hip pain, you may need to see a doctor for further treatment options such as a steroid injection or surgery.
Finally, if a strengthening program and injections don’t work, you may have to consider having a Total Hip Replacement as arthritis has progressed too far.
Hip Flexor Tendonitis
The hip flexor muscles are a group of muscles that allow you to lift your leg and bend your hip. The most common hip flexor muscle is the Iliopsoas, but a handful of muscles on the front of the hip make up the hip flexor muscle group.
Tendonitis of the hip flexor muscles is caused by overuse, repetitive motions, or sudden impact such as a fall. The hip flexors are commonly underworked and weak in people who sit most of the day, such as office workers.
The first symptom of hip flexor tendonitis is typically pain in the front of the hip that is worse with activity such as walking or lifting your leg. The pain is often a sharp, shooting pain that comes on with certain activities. One of the first activities that cause pain is trying to lift your leg up to put on your shoes.
The tell-tell way to diagnose hip flexor tendinitis is to lie flat on your back and try to lift your painful leg off the bed. Especially if the pain started after a recent increase in activity but popping or catching, you can almost be sure.
How to Address Hip Flexor Tendonitis
The first thing you need to do is stop doing the activities that aggravate your hip flexor tendonitis. This will give the tendon time to rest and heal.
Once the pain has subsided, you can start a hip flexor strengthening program to help prevent the injury from happening again. These exercises should be done slowly and progressed gradually over time so that you avoid re-aggravating the injury.
Exercises such as squats and lunges are great to work in addition to a targeted hip flexor strengthening program. Some of our favorite hip flexor strengthening exercises include Straight leg raises and banded hip flexion.

You should also stretch the hip flexors, especially if you notice a reduction in pain after stretching. However, stretching should not be the only activity that you do to address hip flexor tendonitis.
Related Topic: Hip Flexor Tendonitis After a Total Hip Replacement
Hip Labral Tear
The hip labrum is a cartilage ring that sits around the hip socket and helps to stabilize the hip joint. The hip joint needs this extra layer of cartilage for extra stability to keep the ball of the hip from slipping out of the socket.
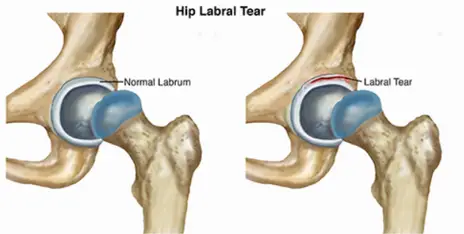
A hip labral tear can happen due to repetitive hip motions, a sudden impact or fall, or prolonged hip impingement called FAI.
The first symptom of a hip labral tear is typically pain in the hip that gets worse with activity such as squatting, lunging, or deep positions of hip flexion.
The pain is often sharp and shoots to the groin region. However, pain in the back of the hip and in the glute region can also be expected.
Catching and grabbing deep within the joint is a very common sign of a labral tear.
To help diagnose a labral tear, try lying on your back and bringing your knee to your chest; once you get there, rotate your foot on the same leg out sideways. You’re looking for a catch, clunk, or reproduction of pain symptoms.
How to Address a Hip Labral Tear
The first thing you need to do is modify or pause the activities that aggravate your hip. This will help reduce the swelling and inflammation within the joint and decrease muscle spasms.
Once the pain has started to subside, you can start walking, swimming, or even try an elliptical program as long as it is pain-free.
A hip strengthening program is essential to ensure that the joint is stable for long-term success. The stronger the muscles around the hip are, the less catching and grabbing inside the joint.
We recommend working the hip abductors, strengthening the glutes, and progressing to more functional exercises like squats and lunges.

One of our favorite exercises is the Bulgarian split squat. This works on many muscles around the hip and builds strength quickly.
Lumbar Radiculopathy
Lumbar radiculopathy is a condition that happens when the nerve roots in your lower back become compressed. This can be from a herniated disc, degenerative changes to the vertebrae in the spine, or due to spinal stenosis.
The first symptom of lumbar radiculopathy is typically pain that radiates down the leg into the buttock and posterior thigh. The pain is often worse with sitting, standing, or walking long distances.
The pain can also be accompanied by numbness, tingling, and weakness in the leg, also called Sciatica.
To help diagnose lumbar radiculopathy, see if you can barely aggravate your symptoms, such as lying flat on your back or sitting in the spot to increase pain. Once you have that slight irritation, perform a pelvic tilt where you rotate the pelvis backward.
If this changes your symptoms, the pain is likely from the back because you haven’t changed anything in the leg or glutes.
You can also see if your Straight Leg Raise range of motion is equal. This test tells you if the nerve roots in the back are irritated.
If the symptomatic side can only raise a little bit compared to the healthy side, this indicates nerve root irritation in the back.
How to Address Lumbar Radiculopathy
The most important thing to do with lumbar radiculopathy is to keep moving! If you become sedentary, the muscle and joints in the back will stiffen up and make this much worse.
We highly recommend walking, swimming, and doing some gentle stretching to maintain your range of motion as you are able.
Aerobic activity such as walking or swimming helps increase blood flow to the area, which will help manage swelling and inflammation.
Stretching is essential to maintain the range of motion in the hips, low back, and legs. We recommend starting with a simple hip stretch called the figure 4 stretch.

If sitting for long periods seems to increase your pain, try using a lumbar support pillow (link) when you have to be in these positions.
We also recommend avoiding high-impact activities or any exercises that require heavy lifting or compression through the spine.
Finally, strengthening the core, glutes, and muscles of the low back is crucial to speed up healing and prevent this from coming back again once it’s all healed.
If this is the cause of your hip pain when you are ascending or descending stairs, there are typically a few modifications that can make a significant difference.
The first is to tighten your abdominal muscles when you are performing stairs. Tighten your stomach by bringing your belly button towards the spine and holding it when you are doing the stairs. This typically does the trick for most people.
The other option that tends to work quite frequently is to change the angle of the back when you are performing stairs. Try leaning a little bit further forward from this waist when the pain takes hold.
If that doesn’t do the trick, try leaning slightly backward at the waist once the pain starts when performing stairs.
Finally, if neither of those positional changes works, try squeezing your glute muscles as hard as you can on the stairs. This braces the pelvis and low back and should give you the stability that you need.
Helpful Tips for Reducing Hip Pain with Stairs
There are many different causes of hip pain with stairs, but they typically all respond to a few other treatments to make your pain go away. These include:
- Increasing your hip and glute strength
- Stretch the deep hip musculature with exercises such as the Figure 4 stretch
- Making small changes in your hip and back angles
- Lead with the other leg until symptoms calm down
- Tighten your abdominal muscles
- Change the angle of your back
- Squeeze your glute muscles when you are on stairs
If you are still having hip pain, it’s essential to consult with a physical therapist to rule out any more serious causes and develop an individualized plan to reduce your hip pain.
Conclusion
Suffering from hip pain can be challenging to deal with when doing the stairs, but you can do a few different things to make it better. If you have hip pain, try some of the tips above and see if they help alleviate your symptoms.
If your pain persists, consult with a physical therapist to rule out any severe causes and develop an individualized plan to help you get back on your feet.
Leave us a comment below if anything was helpful, or you have any other tips for addressing hip pain in general.
Disclaimer: The information provided in this post is for educational purposes only. This is not a substitute for a medical appointment. Please refer to your physician before starting any exercise program.
