Cervicogenic Headaches
 Many of us have experienced episodes of headaches throughout our lifetime, ranging from a mild nuisance to severe pain. There are several different kinds of headaches, depending on the origin of the pain. A cervicogenic headache (CGH) is a specific type of chronic headache that affects between 0.4 – 2.5% of the general population.1 The average age of patients with this condition is 42.9 years, and it appears to be more prevalent in women.1 Although the causes of the condition are ambiguous, what is certain is that patients with CGHs experience a significant loss of functioning and debility due to their pain.1 It is important to understand how a CGH may arise and the ways in which to both prevent and manage the pain.
Many of us have experienced episodes of headaches throughout our lifetime, ranging from a mild nuisance to severe pain. There are several different kinds of headaches, depending on the origin of the pain. A cervicogenic headache (CGH) is a specific type of chronic headache that affects between 0.4 – 2.5% of the general population.1 The average age of patients with this condition is 42.9 years, and it appears to be more prevalent in women.1 Although the causes of the condition are ambiguous, what is certain is that patients with CGHs experience a significant loss of functioning and debility due to their pain.1 It is important to understand how a CGH may arise and the ways in which to both prevent and manage the pain.

What Are Cervicogenic Headaches?
What are CGHs?
Cervicogenic headaches (CGHs) are secondary headaches, meaning that they are a result of an underlying condition.2 Clinicians will often label this as “referred pain,” since the origin of the pain “refers” the discomfort to a separate area of the body.1 In this case, a CGH is a head pain that is referred from bones or soft tissues in the neck.1 This may be due to previous neck injury, musculoskeletal dysfunction, or muscle imbalances.2 To understand how abnormalities in our neck can even translate into a pain in our head, we must first take a look at the anatomy of the neck and spine. 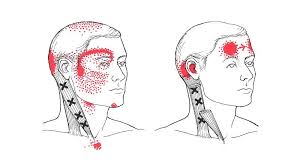
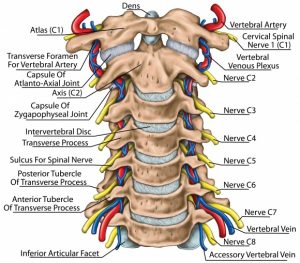
Anatomy of the Neck and Causes of CGHs
The spine is anatomically partitioned into three major sections – the cervical, thoracic, and lumbar spine.3 Each of these sections consists of individual bones, called vertebrae, stacked on top of each other, with fibrous discs in between each.3 The cervical spine is the uppermost portion of the spine and is made of 7 cervical vertebrae, which are located at the base of the skull where our neck is located.3 Each of the vertebrae has spinal nerves that carry sensory information to and from the spine, with the upper three cervical spinal nerves (C1-C3) relaying pain signals to the pain center of the head and neck to – the Trigeminocervical Nucleus.4 Not only does this pain center receive information from the cervical spine, but it also relays sensory information to the head and neck.1 It is this functional convergence that is thought to account for the referral of pain between the neck and the face/head in a CGH.1 After sustaining neck trauma, whiplash, concussions, or chronic neck strain/spasms can result in dysfunction to the neck musculature, thereby precipitating a CGH.5
Symptoms and Diagnosis
The diagnosis of a CGH is no easy feat since its symptoms closely mimic those of primary headaches (headaches that are not a result of other conditions) and migraines. However, there are some characteristic features of a CGH that may set it apart from other similar syndromes.
- A CGH usually presents as chronic, deep, non-throbbing head pain, while the neck pain is described as a tightness or stiffness.1
- This pain is often worsened by specific neck movements or sustained posture and may result in a limited range of motion of the neck.4
- As with other types of headaches, this particular syndrome may be associated with nausea, vomiting, light/sound sensitivity, and/or dizziness.1
- With all of this in mind, the basic criteria to differentiate these symptoms from other headaches/migraines is the origin of the pain – diagnosis of a CGH must involve the source of the pain be in the neck, with the pain being perceived in the head/face.5 Other types of headaches will not have their origin in the neck.5 To clearly differentiate the conditions, clinicians may choose to blockade specific facial/spinal nerves – if this intervention relieves the associated pain, a definitive diagnosis of CGH can be made.5
Do you have frequent headaches? Have you tried a Home Cervical Traction Unit? See our reviews of the Best Home Traction Units to Decrease Pain and Improve Mobility
Treatment Options
Though some clinicians choose to begin treatment with medical management, CGH patients frequently do not significantly respond to medications alone.1,6 More invasive procedures can be used, such as occipital nerve blocks, anesthetic blockades, and treatment with radiofrequency energy, but due to their associated risks and uncertain outcomes, most CGH treatment options begin with conservative interventions.2,5 Thus, a multi-modal approach involving manipulative therapy and therapeutic exercise is usually the first-line treatment for patients.2,5 In one controlled study, patients experienced a significant reduction in headache frequency and intensity after adhering to a 6-week treatment regimen of manipulative therapy and an exercise program.7 These physical treatment modalities are most effective for preventing and controlling headaches when patients are involved in ongoing exercise and physical conditioning programs combined with gentle stretching.1,8
In other words: regular exercise is key! With this in mind, we’ve compiled several of our favorite exercises below to help you better manage your headaches at home, whether they be a CGH or other primary headaches.
Exercises to Help Reduce Headaches
Upper Trap Stretch
Goal: Loosen the muscles of trapezius to relieve neck, shoulder, and upper back pain
Instructions:
- Sitting down, place the arm you want to stretch underneath your seated leg, to hold the shoulder down
- Alternatively, you can consciously extend your arm to hold the shoulder down
- With your free hand, gently tilt your head away from the designated shoulder
- Hold the stretch for a minimum of 30 seconds
Cervical SNAGs
Goal: To reduce upper neck tightness and stretch the upper trapezius muscles, which will enhance side-to-side neck rotation
Instructions:
- Roll up a towel and drape it around your neck
- Hold both ends of the towel with your hands.
- Use your right hand to anchor that end of the towel to your body. Try to keep this end still.
- With your left hand, bring the other end of the towel to eye level keeping the towel taught
- Slowly turn your head to the right until you begin to feel tightness in the neck
- Make sure your chin stays level and does not lift upwards. Imagine touching your chin to your shoulder
- Once you feel neck stiffness, use the left hand and towel to coax the head to turn even further
- Repeat several pulses, then proceed to stretch the other side of the neck
Chin Tuck and Lift
Goal: Bring balance to the head and neck, realigning your head with your shoulders. This will decrease strain on the neck
Instructions:
- Lay down on a bed or table with your head gazing at the ceiling
- Without lifting your head off the table, tilt your chin down until it meets your neck
- Now, slowly lift your head a few centimeters off the bed
- Hold this position for 10 sec, then release
- Return to starting position and repeat 10x/day
Open The Book – Thoracic Rotation
Goal: To improve thoracic rotation and help the whole upper spine rotate
Instructions:
- Begin lying on your side
- Place both arms in front of you at a 90-degree angle with your torso, have your palms touching each other
- Position your top knee on a foam roller or ball
- Keep this knee in contact with the foam roller/ball throughout the exercise
- Inhale deeply
- With the inhalation, keep your top arm extended/lengthened and circle it up and over your body until it reaches the opposite side of the floor
- Imagine drawing a half-circle in the air with your arm
- Twist your torso with the arm movement
- Exhale and bring your arm back to starting position
Prone Chin Retractions
Goal: Promote extension of the neck to activate deep cervical flexor muscles. This will increase cervical spinal strength and range of motion
Instructions:
- Lay on your stomach on a bed or table, with your head slightly off the edge
- Slowly retract your head by pulling your chin up towards the ceiling
- Hold for 5 seconds
- Release to neutral
- Repeat several times
Other Helpful Tips For Headaches
Stay Hydrated
Many have probably heard the popular wisdom that drinking water can stave off headaches. While increasing fluid intake may not decrease the number of headache episodes, it has been shown to modestly reduce the intensity or duration of the pain.9,10 Because many headaches can be linked to dehydration, it is reasonable, low-risk, and cost-effective to try increasing your water intake and noting whether you experience improvement in symptoms. Needless to say, drinking more water is sure to have other positive benefits on your overall health, regardless if dehydration is the cause of your headaches.
Exercise Regularly
Exercise is critical for the overall prevention and management of most chronic conditions, including headaches.11 The problem some patients may face is that exercise can exacerbate their migraine/headache symptoms, deterring them from exercising at all.12 However, the research overwhelmingly supports the use of physical activity as a preventative and acute treatment for migraines and headache, having beneficial effects on frequency, duration, and associated disability.11,13 When intentionally incorporated into a regular routine, small amounts of aerobic exercise can have a positive effect on headache prevention and management in the long term.12
Use Heat to Reduce Muscle Tightness
For years, cryotherapy (the therapeutic use of cooling/freezing temperatures) was thought to be most helpful for treating injuries and muscle soreness.14 Over time, though, we have begun to see that thermotherapy (the therapeutic use of heat/hot temperatures) may be more effective in healing specific injuries.15 Using heat packs increases blood flow to the area and improves tissue metabolism/stretchability.15 In general, placing hot packs on the neck/shoulders can help to minimize neck stiffness and improve mobility.
Reduce Stress
We get it – this is much easier said than done. In fact, headache/migraine sufferers report stress to be the primary trigger for their attacks.16 The pain intensifies, causing them even more stress and leading to a vicious cycle of increased headache frequency.16 Without intentional stress management intervention, this stress can feed chronic headaches indefinitely. It comes as no surprise, then, that stress management and relaxation therapies (in combination with other physical and mental therapies) have been shown to significantly improve pain intensity, duration, and related disability.17 It goes without saying that stress management plays an important role in every aspect of life but is especially important for headache management.
Conclusion
While CGHs often go misdiagnosed or even undiagnosed, the importance of identifying and treating this condition cannot be understated. Fortunately, there are effective ways to do so at home with a physician’s oversight. We hope that this knowledge and our recommendations can help you to begin living a life headache-free!
Works Referenced:
- Biondi, D. (2005). Cervicogenic Headache: A Review of Diagnostic and Treatment Strategies | The Journal of the American Osteopathic Association. The Journal of American Osteopathic Association 105.
- Page, P. (2011). Cervicogenic headaches: an evidence-led approach to clinical management. International Journal of Sports Physical Therapy 6, 254–266.
- Anatomy of the Spine. (2020). Southern California Orthopedic Institute. Retrieved from https://www.scoi.com/specialties/spine-doctor/anatomy-spine.
- Cervicogenic Headache. (2020, February 4). Physiopedia. Retrieved from https://www.physio-pedia.com/index.php?title=Cervicogenic_Headache&oldid=229653.
- Al Khalili, Y., and Murphy, P.B. (2018). Cervicogenic Headache (StatPearls Publishing).
- Bogduk, N., and Govind, J. (2009). Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. The Lancet Neurology 8, 959–968.
- Jull, G., Trott, P., Potter, H., Zito, G., Niere, K., Shirley, D., Emberson, J., Marschner, I., and Richardson, C. (2002). A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 27, 1835–1842.
- Biondi, D.M. (2005). Physical treatments for headache: A structured review. Headache 45, 738–746.
- Spigt, M.G., Kuijper, E.C., Van Schayck, C.P., Troost, J., Knipschild, P.G., Linssen, V.M., and Knottnerus, J.A. (2005). Increasing the daily water intake for the prophylactic treatment of headache: A pilot trial. European Journal of Neurology 12, 715–718.
- Spigt, M., Weerkamp, N., Troost, J., van Schayck, C., and Knottnerus, J. (2012). A randomized trial on the effects of regular water intake in patients with recurrent headaches. – PubMed – NCBI. Family Practice 4, 370–375.
- Daenen, L., Varkey, E., Kellmann, M., and Nijs, J. (2015). Exercise, not to exercise, or how to exercise in patients with chronic pain? Applying science to practice. Clinical Journal of Pain 31, 108–114.
- Amin, F.M., Aristeidou, S., Baraldi, C., Czapinska-Ciepiela, E.K., Ariadni, D.D., Di Lenola, D., Fenech, C., Kampouris, K., Karagiorgis, G., Braschinsky, M., et al. (2018). The association between migraine and physical exercise. The Journal of Headache and Pain 19, 83.
- Domingues, R.B., Teixeira, A.L., and Domingues, S.A. (2011). Physical practice is associated with less functional disability in medical students with migraine. Arquivos de Neuro-Psiquiatria 69, 39–43.
- Galbraith, R.M., and Lavallee, M.E. (2009). Medial tibial stress syndrome: Conservative treatment options. Current Reviews in Musculoskeletal Medicine 2, 127–133.
- Nadler, S.F., Weingand, K., and Kruse, R.J. (2004). The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician 7, 395–399.
- Sauro, K.M., and Becker, W.J. (2009). The stress and migraine interaction. Headache 49, 1378–1386.
- Lemstra, M., Stewart, B., and Olszynski, W.P. (2002). Effectiveness of multidisciplinary intervention in the treatment of migraine: A randomized clinical trial. Headache 42, 845–854.
Disclaimer: The information provided in this post is for educational purposes only. This is not a substitute for a medical appointment. Please refer to your physician before starting any exercise program.